In 2023, the Sydney Pharmacy School implemented a new vertically integrated curriculum. Incoming first-year students enrolled in the Pharmaceutics and Pharmacy Practice (PHAR1921) unit of study will undertake a week-long placement in a community pharmacy and will be tasked with counselling a patient about a simple ailment that draws on the use of non-prescription medicines. The goal is to not only develop students’ communication skills but also to develop their breadth and depth of therapeutic knowledge on core areas that they are likely to encounter during placement. An obvious choice would be to make use of clinical role plays adopting a case-based learning approach. Clinical role plays form an important part of the pharmacy curriculum, simulating real-world patient interactions and putting the student into the shoes of the pharmacist. While a typical encounter lasts about 5 minutes, the interaction is complex, requiring the pharmacist to gather information from the patient, analyse this information and provide a suitable recommendation that is then communicated to the patient.
Education Challenge
Pre-work completed before class aims to provide the learner with foundational knowledge. But like many other disciplines at the University, we also struggle to get students to complete assigned readings and pre-work before class. Similar units would often set pre-work as submitted Canvas assignments, taking 1-2 hours for tutors to mark. At best, these pre-work tasks are completed at a surface level by simply ‘copying and pasting’ content to answer questions. Notwithstanding issues of academic integrity, students might not get a chance to properly understand and consolidate information they had just read. As a result, a large portion of class time is spent addressing students’ knowledge gaps, while running out of time to complete the core active learning activities in class.
Importantly, without this foundational knowledge, students often arrive in class unprepared to participate in the counselling role plays, which call for higher-order thinking (application, analysis, evaluation and creation). After all, the quality of counselling is dependent on how well students know and can apply the clinical recommendations and guidelines to the presenting patient. Additionally, we need to professionally socialise first year students into the pharmacy profession by helping them to acquire pharmacists’ ways of thinking and ways of doing – from the vocabulary of technical terms and navigating drug information sources, to grasping the practice norms of the profession. Having been involved in teaching first-year pharmacy students over the last few years and adapting transitional activities into pharmacy, the new curriculum was an opportunity to re-think transition and professional socialisation in tandem.
Education Design Rationale
As part of PHAR1921, students are tasked to look after a hypothetical family over the course of the semester, managing various ailments including parasitic infections, cough and cold, paediatric medicine, gastrointestinal health, and skin health, in preparation for their upcoming clinical placements in community pharmacies. Clinical case studies are built around the Wattle family and their pet dog, allowing students to make clinical decisions that consider the family’s existing medication/medical history. The continuous structure aims to build a clinical narrative to humanise the case studies, to allow students to engage and look after different family members as their clinical trajectories unfold over the semester, rather than using disparate case studies over the semester.
This education design aims to scaffold learning and help students gain mastery of threshold concepts within a therapeutic topic in an authentic way. These threshold concepts might relate to common drug interactions or precautions to take for patients with specific comorbidities. Each learning activity in the workshop was designed to expose and reinforce students’ understanding of these threshold concepts. Activities are scaffolded with increasing levels of complexity, starting from simple awareness of assigned readings, to interpretation of information in the quiz, followed by synthesis and application during the role plays.
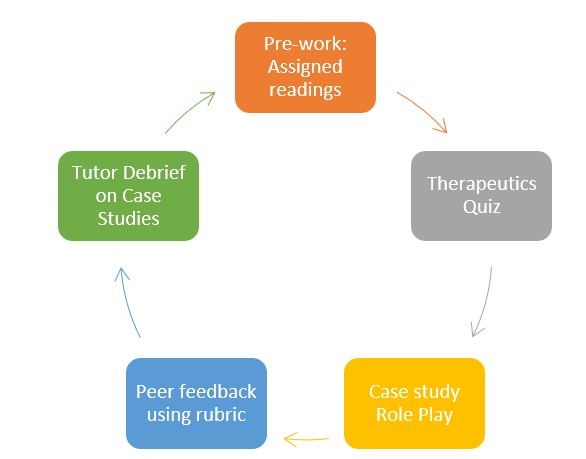
Step 1: Assigned Pre-Readings
In the first four weeks of semester 2, students participate in a range of foundational skills workshops such as communication skills, professional ethics, and dispensing skills to prepare for clinical encounters and role plays. Building on these foundational skills, from week 5 of semester students are given assigned readings from the Australian Medicines Handbook, an independent, evidence-based, national drug reference, accessible through the Library e-resources, along with a series of pre-work questions that are designed to guide their reading in preparation for the quiz. Based on the therapeutic area, a series of short and concise e-book sections (30–40-minute read) were chosen to not overwhelm students, as the volume and content complexity often deter students from starting in the first place.
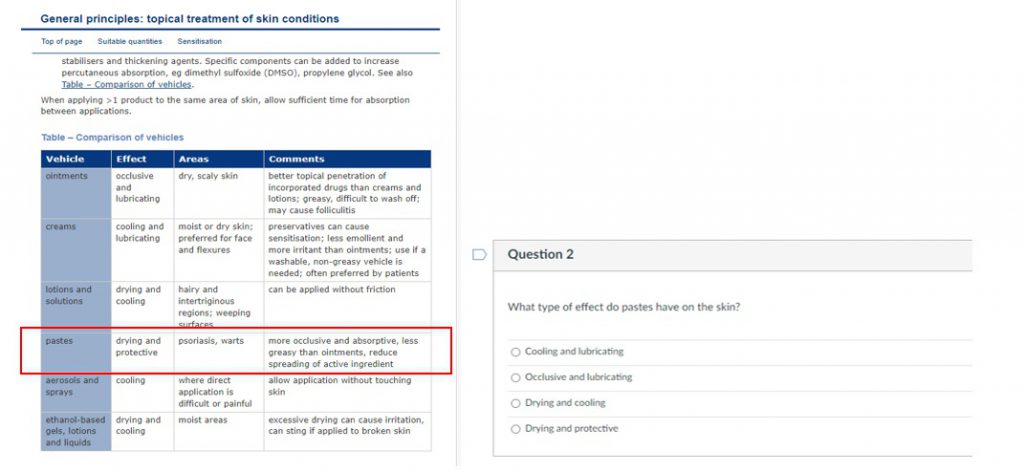
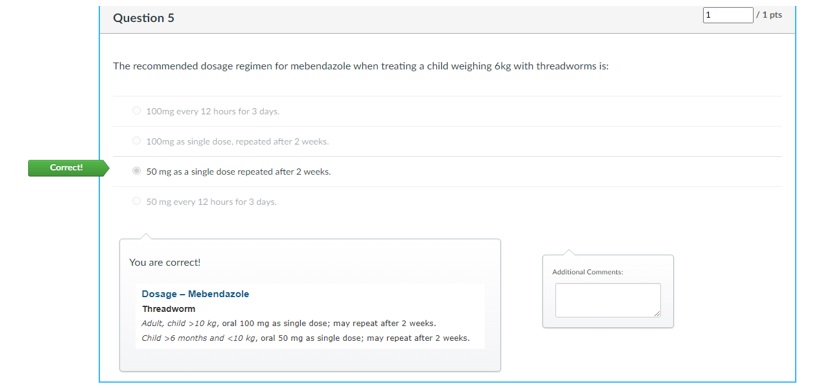
Step 2: Restricted Open-book Therapeutics Quiz
In the following week, students complete a restricted open-book therapeutics quiz (8 questions) on Canvas in the first 15 minutes of class, worth 2.5% of the unit’s overall mark. To ensure academic integrity, the quiz draws from a bank of questions with 4-5 variations per question that are comparable in difficulty. Students are asked not to memorise information, as the quiz will focus on drug information navigation and interpretation. The goal of the quiz questions is to mimic the real-world requests that pharmacists encounter in practice, ensuring students engage with key threshold concepts as part of their assigned readings and quiz-taking.
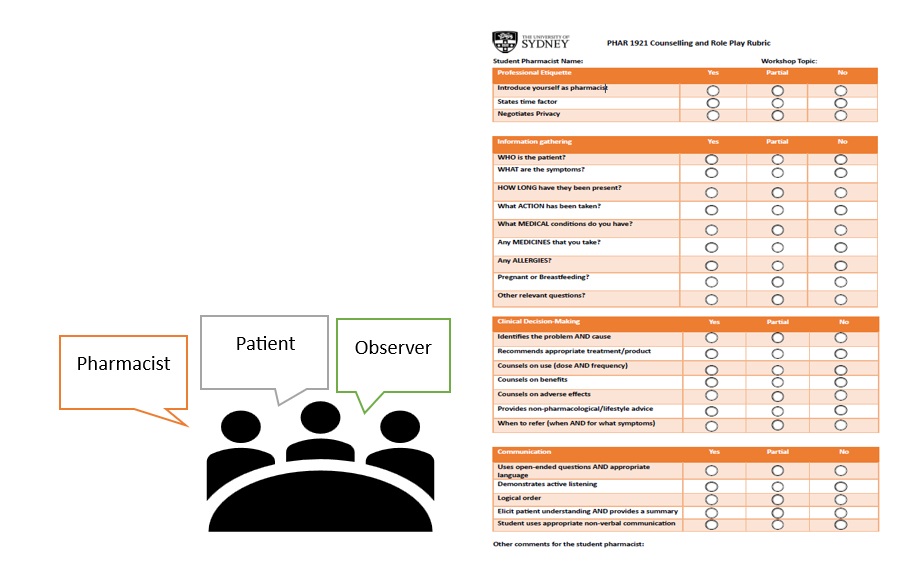
Step 4: Clinical Role Play, Peer Feedback and Tutor Debrief
Following the quiz, students take part in a case study role play. This portion of the workshop addresses three core case studies, drawing on the threshold concepts that are covered in the pre-work readings and quiz questions. The education design extends from a first-year unit of study in the old curriculum, Pharmacy Practice 1 (PHAR1821), where students work in groups of three: one student being the pharmacist, one being the patient offering information to the pharmacist and one being the observer, peer-assessing the performance of the student pharmacist against a marking rubric. The role play is followed by peer feedback and a class debrief by the tutor. Following each case study, students rotate roles and take turns in playing the pharmacist, patient, and observer at least once in each workshop.
Step 5: Timely Quiz Feedback
Once the last workshop group of the week completes the quiz, student grades, and feedback are released by Friday afternoon. Feedback is provided in the form of a screen capture to allow students to directly see how the quiz questions relate to their assigned readings. Given the large cohort size, the technological affordances of Canvas enable timely feedback to be fed forward to students before their next quiz the following week, giving them the chance to reflect on their learning and apply their learning to future weeks.
Impact and Results
Over the course of Semester 2, students engaged in five cycles of learning according to this workshop format. Using the therapeutics quiz as a proxy measure for pre-work completion, the average marks across the cohort over the five quizzes was 90%, which meant students were on average getting 7 out of 8 questions correct per quiz. This suggests a high level of student engagement with pre-work readings since answers to questions come directly from the assigned readings in the Australian Medicines Handbook.
From the students’ perspective, their quiz performance provided a source of positive reinforcement that motivated them to complete the next set of readings in the subsequent week. Importantly, over the course of semester, students began to realise the value proposition of completing their pre-work readings – a greater depth of understanding in the respective therapeutic areas. Students commented on feeling better prepared and more confident during the information gathering and counselling as the student pharmacist. Similarly, the observers became more attuned with what to look out for and provided relevant constructive feedback (what’s missing or not), while those acting as the patient were more astute in their responses to the student pharmacist.
After completing the readings and quiz, the case studies connect, and I feel I understand the topic better and I become more confident in the information gathering and counselling
I liked the quiz because as you look for the information to answer the quiz questions, you end up learning about other information in passing
From tutors’ perspective, the current workshop format not only overcame the barrier of getting students to do pre-work but also facilitated their teaching practice. The time not spent on re-teaching pre-work materials opened new opportunities and time for tutors to draw on their real-world clinical experiences during the debrief.
It empowers students with foundational knowledge to navigate the complexities of therapeutic practice with confidence and serves as a coherent guide for our group discussions. As an instructor, my experiences have shown me that this approach cultivates a deeper understanding and meaningful engagement, fostering a rich and dynamic learning environment.
Final Thoughts
Sometimes getting started is the hardest part of learning for students. Through setting relatively low-stakes assigned readings and associated assessment tasks, students saw a direct alignment between class exercises and assessment. The focus became knowledge attainment rather than differentiating between students. This approach arguably boosted student confidence in task completion while consolidating necessary threshold concepts.